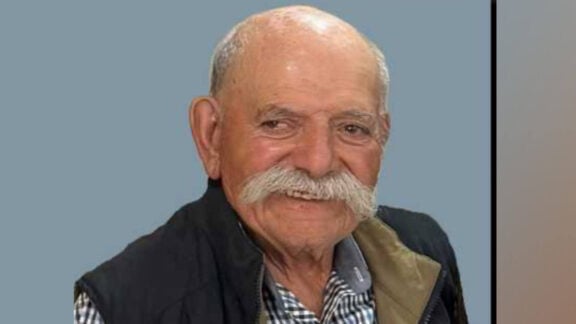
Professor Arthur (Athanasios) Christopoulos, Dean of the Faculty of Pharmaceutical Sciences at Monash University, is at the centre of a significant discovery that promises to bring radical changes to the treatment of schizophrenia.
Following the recent approval of the drug Cobenfy by the US Food and Drug Administration (FDA), Professor Christopoulos spoke to Neos Kosmos about how this new medication can significantly improve the lives of patients.
A novel approach to schizophrenia treatment
What makes Cobenfy, previously called KarXT, stand out from earlier antipsychotic drugs is its innovative approach to treating schizophrenia. Unlike traditional antipsychotics, which have been used since the 1950s and primarily work by blocking dopamine receptors in the brain, the new drug targets a different brain chemical.
“It is the first antipsychotic drug with a completely different mechanism of action compared to all previous drugs,” explains Professor Christopoulos.
“All antipsychotics to date act on a brain chemical called dopamine and block it. However, this drug works on a completely different brain chemical.”
Cobenfy has fewer and milder side effects compared to existing drugs.
“It’s cleaner,” he says. “It has a different side effect profile that is not as severe as current medications.”
Hope for treatment-resistant patients
One of the most important features of Cobenfy is its potential to help people with schizophrenia who do not respond to any existing treatments.
“About 30 per cent of people with
schizophrenia don’t respond to any drug,” Christopoulos notes.
“Now we at least have a new type of drug that these individuals who don’t respond can try.”
Cobenfy’s promise, however, doesn’t stop there. The drug also has the potential to improve symptoms beyond psychosis, something current medications struggle to do effectively.

“Schizophrenia is not just psychosis—it has other symptoms as well. Many people experience emotional withdrawal. Many have memory problems. Existing medications don’t address these issues. Cobenfy has the potential to treat them,” Christopoulos says.
The professor believes it is still too early to determine whether the new medication will primarily be used as a monotherapy or in combination with other antipsychotic drugs.
“We will likely see both,” he explains. “Doctors will initially try it on its own, but I believe in the future we will see it combined with other medications to reduce the dose of older drugs and minimise side effects.”
A challenging road to success
Professor Christopoulos’s involvement with the approved FDA drug goes back to the 1990’s when his PhD research into areas of the brain coincided with similar research with scientific colleagues overseas. He developed an ongoing collaboration with both scientists and the pharmaceutical companies involved over the decades.
It would not be an understatement to say that without Christopoulos and the considerable efforts across multiple academic groups, including key groups in Australia like the Monash Institute of Pharmaceutical Sciences, and the Florey Institute of Neuroscience and Mental Health, Cobenfy would not have come to fruition.The development of Cobenfy was a long journey filled with challenges, requiring nearly 30 years of collaboration between academia and the pharmaceutical industry. Initially discovered as a treatment for Alzheimer’s disease, clinical trials did not show significant results in patients. However, some of those who exhibited psychotic symptoms saw improvement, which inspired the idea of testing the drug for schizophrenia.
Convincing stakeholders to invest in a drug that had already failed in one area wasn’t easy.
“The first challenge was getting people to believe that this different hypothesis—that we can target different brain chemicals and proteins—might work for schizophrenia,” says Professor Christopoulos. “Many didn’t believe it.”
Another challenge was reformulating the drug.
“It’s actually a combination of two drugs,” he explains, adding that one was initially tested for Alzheimer’s, but another was added to reduce side effects. “This was the second challenge—the reformulation.”
New horizons
Although the approval of Cobenfy marks a significant milestone, Professor Christopoulos stresses that the research is far from over.
“Cobenfy clinically confirms that the brain proteins and chemicals we study have an impact on schizophrenia. However, these proteins also play a role in treating other conditions, such as Alzheimer’s, Parkinson’s disease, and even pain,” he explains.
“We are expanding our research to see how we can develop even cleaner, more selective drugs for a broader range of conditions.”
For those living with schizophrenia, the approval of Cobenfy signals a new era.
“Antipsychotic medications have been around since the 1950s, but they’ve been largely the same type of drug with small variations. Cobenfy is an entirely new kind of drug that will help patients who don’t respond to existing antipsychotics,” Christopoulos adds.
Looking to the future, the professor remains optimistic.
“This is only the beginning,” he states, predicting a future where more effective, targeted treatments for various mental disorders become a reality.
For now, the FDA approved drug promises to opens new horizons, not only for those living with schizophrenia but also for the broader scientific community researching neurological and psychiatric disorders.
In Australia the medication will need Therapeutic Goods Administration approval before becoming available, and its price may be a barrier to access without PBS listing.